Addiction affects so many aspects of a person’s life. Our approach to treating the needs of each individual person is the key to a successful outcome. At Crossroads Centre Antigua, we aspire to help our clients live a substance free life – free of opioids and other mood altering drugs. Another aspect of this approach is to provide continuing education so that you may be informed of the world around you when it comes to staying in recovery.
In the news, we’ve heard about the opioid epidemic, and the mere word “epidemic” is frightening. It is because opioids have become a mainstay in pain treatment, yet these drugs are highly addictive. For someone in recovery, we want you to understand opiates and how to combat them in order to maintain your healthy lifestyle.
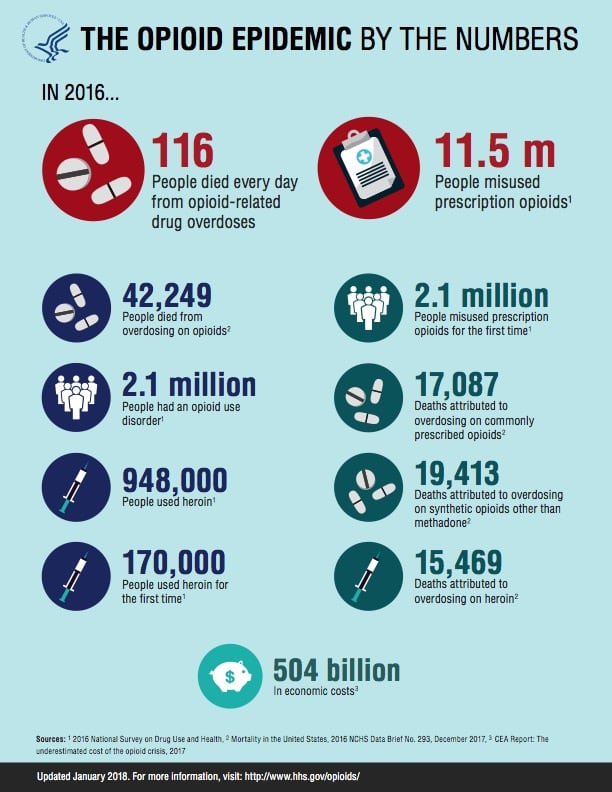
Let’s take a look at the alarming statistics: every eight minutes a person dies from the cycle of opioid addiction. With 175 deaths every day, the United States has seen a 400% rise in opioid addiction and overdose since 2000. It is estimated that 2 million Americans have become dependent or abuse prescription pain pills and street drugs. Furthermore, among the 630,000 people who have died from a drug overdose between 1999 to 2016, approximately 66% of the more than 63,600 drug overdose deaths in 2016 involved an opioid.
These startling statistics simply scratch the surface on the opioid crisis.
So how did we get here? We will start with the history of these drugs, what is happening to combat them and delve into understanding the nature of their addiction.
Living with chronic pain can be devastating, and effective pain management is important to getting one’s life back. While doctors discussed treatment options, some medications, such as prescription opioids, have been found to relieve pain in the short term. In the late 1990’s, the benefits seemed to outweigh the risks. Healthcare providers began to prescribe them at greater rates. Increased prescription of opioid medications led to widespread misuse of both prescription and non-prescription opioids before it became clear that these medications could be highly addictive, even deadly.
According to the Centers for Disease Control and Prevention, “there have been three distinct waves in the rise of opioid overdose deaths. Beginning in the 1990’s, there was an increase in prescribing opioids. Rates of overdose deaths involving prescription opioids (natural and semi-synthetic opioids and methadone) have increased since at least 1999. The second wave began in 2010, with rapid increases in overdose deaths involving heroin. In 2013, the third wave began showing significant increases in opioid overdose deaths involving synthetic opioids, particularly illicitly manufactured fentanyl (IMF). From 1999 to 2016, more than 630,000 people have died from a drug overdose. In 2016, 66% of those (63,600) involved an opioid, which shows the growth being five times higher than in 1999.
Opioid misuse and abuse have caused US leaders and health care specialists to take a stand and wage war on this epidemic.
In 2017, the US Department of Health and Human Services (HHS) declared a public health emergency and announced a 5-Point Strategy to Combat the Opioid Crisis:
-
Improving access to treatment and recovery services
-
Promoting use of overdose-reversing drugs
-
Strengthening our understanding of the epidemic through better public health surveillance
-
Providing support for cutting edge research on pain and addiction
-
Advancing better practices for pain management.
This crisis also requires continuing public health education. Policy changes that help eliminate barriers to treatment must happen within our governments. With everyone on the same page, significant progress can be made to deescalate this epidemic.
To better understand this epidemic, now let’s look at what an opioid is, why people are prone to fall victim to these prescriptions, as well as the nature of their misuse.
What is an opioid? These drugs are formulated to replicate the pain reducing properties of opium. They include both legal painkillers like morphine, oxycodone, or hydrocodone prescribed by doctors for acute or chronic pain, as well as illegal drugs like heroin or illicitly made fentanyl. This class of drugs bind to receptors in the brain and spinal cord, disrupting pain signals by releasing the hormone dopamine, creating a feeling of euphoria or a “high.”
Are there different types of pain? The answer is yes: acute and chronic pain. Acute pain usually starts suddenly and has a known cause, like an injury or surgery. It normally gets better as your body heals. Chronic pain is pain lasting three months or more and can be caused by a disease or condition, injury, medical treatment, inflammation, or even an unknown reason.
What are the most common reasons for misuse of a prescription pain reliever? They include:
-
to relax or relieve tension
-
to experiment or see what the drug is like
-
to feel good or get high
-
to help with sleep
-
to help with feelings or emotions
-
to increase or decrease the effects of other drugs
-
because the respondent is “hooked” or has to have the drug
What can you do to prevent opioid misuse? When having surgery or a procedure that would require having an addictive substance, let your doctor know that you are in recovery from addictive substances. Work with your doctor to create a plan on how to manage your pain. Know your options and consider ways that do not include opioids. Talk to your doctor about any and all side effects and concerns. Make the most informed decision with your doctor and follow up regularly.
Engage with your sponsor on a plan of action when having surgery or a procedure done. Don’t keep any secrets. Have a supportive friend or loved one “monitor” your prescription for pain (if needed) for several days until you can start on a non-addictive alternative to pain relief.
Finally, how do you recognize an opioid overdose? It can be difficult. If you aren’t sure, it is best to treat the situation like an overdose—you could save a life. It is important that you don’t leave the person alone, and make sure you call 911 or seek medical care for the individual. Signs may include any of the following:
-
Small, constricted “pinpoint pupils”
-
Falling asleep or loss of consciousness
-
Slow, shallow breathing
-
Choking or gurgling sounds
-
Limp body
-
Pale, blue, or cold skin.
To combat this public health crisis, everyone must learn more about opioids in order to protect yourself and your loved ones from opioid abuse, addiction and overdose.


Paula Hicks says:
I’m a past patient who is still on pain treatment ,, my doctor and I are discussing to go to Medical Marjuana with hopes of getting off of pain meds.,, in another treatment they had me start suboxone which did help but my stomach couldn’t take it,,, addict or not,, some of us have to have help,,, tho you at my time there thought otherwise,,, thought I should leave my husband husband also at the time,, he is probably the best thing for me,, 34 yrs. later,, so I’m confused,, and try to be the best person I can be,, with limits still but couldn’t do anything without the help of my pain Dr., and the medications that keep my pain levels to a point to where I can have some type of life with my family.
rachel frampton says:
I agree with you that Opioid could be used for relaxation and insomnia; maybe that’s why it could be quite addictive. My sister got addicted to Opioid ever since she had to take it to ease the pain after her car accident. Therefore, we have decided to start looking for a health care service that offers addiction treatment. http://winchesterrecovery.com/